COVID-19 has devastated the U.S., and the loss of lives won’t stop until hundreds of millions of people are vaccinated in 2021. But during this terrible year, there’s been a bright spot: Businesses and designers working, improvising, and innovating to help as many people as fast as possible.
Let’s be clear, the scale of the pandemic represents a total failure by the U.S. government, which should have contained the spread and organized a proper response. But the efforts of designers, researchers, and even the private sector to come up with solutions in the face of such tragedy is a testament to human resilience and ingenuity. Here are some of the year’s most incredible innovations around COVID-19.
Racing to build better PPE
Early in the pandemic, doctors and nurses ran out of personal protective equipment such as face shields and N95 masks. The sheer innovation that went into mask-making is too much to document. The mask was the design object of the year.

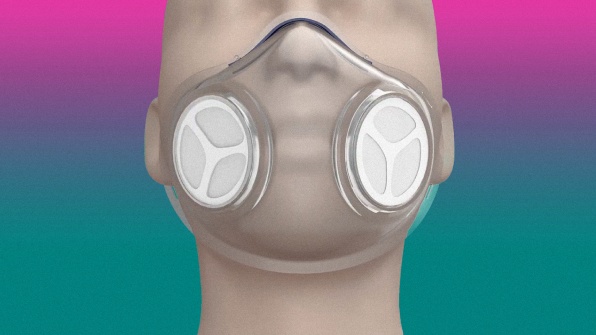
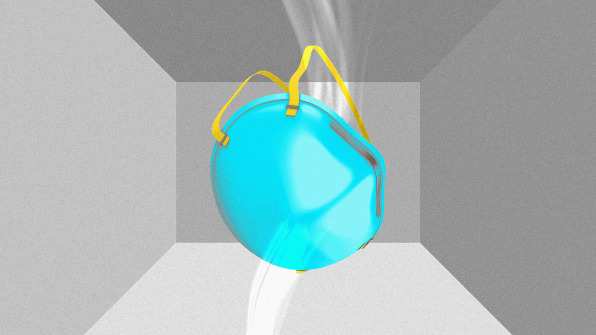
Reusing disposable masks
Manufacturing more PPE was just part of the story, though. Quickly, researchers brought disposable PPE into the lab to figure out if it was possible to reuse it instead of throwing it away. What they discovered again and again was that one-use products were actually viable for a lot longer than anyone had ever thought or tried.
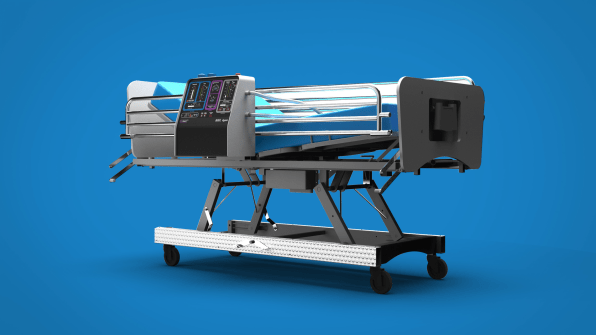
Building new ventilators, fast
As the worst cases of COVID-19 affect one’s lungs and breathing, ventilators can offer a last-ditch possibility for survival and recovery. But even a major city might have only a few dozen ventilators at its disposal. So, much like PPE, governors raced to acquire ventilators early in the pandemic.
Rethinking the hospital
What is healthcare during a pandemic? During COVID-19, it could no longer be about seeing a doctor in a hospital room.
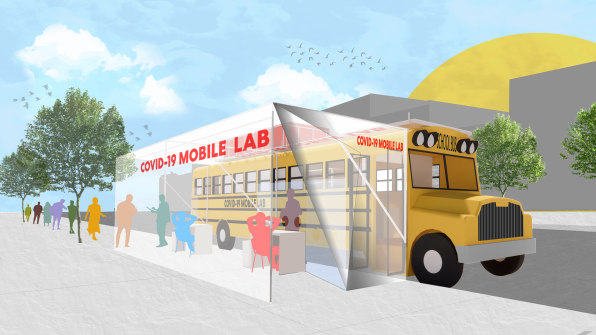
Meanwhile, hospitals had to change approaches to triage on the fly. At Mount Sinai Hospital in New York, doctors wore GoPros to give designers socially distanced walk-throughs of the space. This helped designers create safer floor plans; using simple tape and vinyl coverings, they turned white rooms into clearly delineated zones for COVID-19 care.
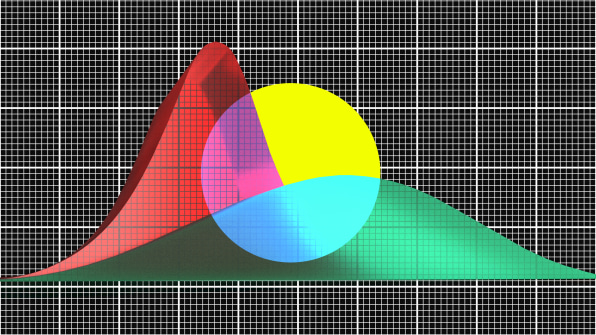
Ushering in a golden age of data and data visualization
Big data has been an empty phrase for years. But data collection and visualization has proven essential during the pandemic, for health officials to track the virus that causes COVID-19 and for the public to understand it.
Our #FlattenTheCurve graphic is now up on @Wikipedia with proper attribution & a CC-BY-SA licence. Please share far & wide and translate it into any language you can! Details in the thread below. #Covid_19#COVID2019#COVID19#coronavirus Thanks to @XTOTL & @TheSpinoffTVpic.twitter.com/BQop7yWu1Q
— Dr Siouxsie Wiles (@SiouxsieW) March 10, 2020
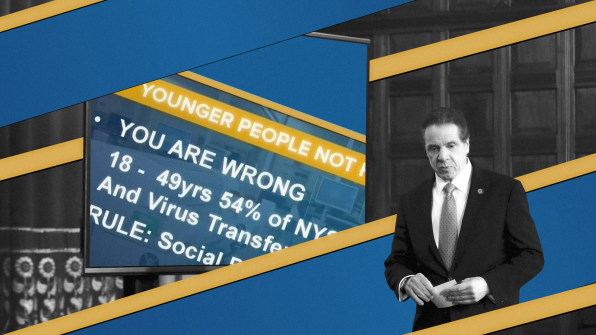
Meanwhile, the field of data visualization flourished. A viral comic strip became an early demonstration of how to share public health information to “flatten the curve” without a frenzy. New Zealand created a superb landing site for the country’s COVID-19 response, complete with a color-coded system to let the public know how socially distanced they needed to be at any given time. Pentagram created a hopeful spin on the pandemic, visualizing all sorts of positive things that have come from it. New York Governor Andrew Cuomo did more with less, leveraging humble PowerPoint slides for his frank informational briefings. And The New York Timesdedicated its entire front page to mark the loss of 100,000 Americans to COVID-19. Unfortunately, U.S. deaths have tripled since then.

The rise of nonhuman helpers
Medical staffing has been in short supply during the pandemic, so much so, that many doctors and nurses have come out of retirement to help. But every time a healthcare practitioner comes into contact with a COVID-19 patient, there’s an inherent risk of infection.

The other solution we’ve seen is to remove humans from the equation altogether. The Taiwanese company Brain Navi retrofitted a one-armed robot to take nasal swabs safely. At Brigham and Women’s Hospital in Boston, Spot, a Boston Dynamics robot dog, was configured to walk into patient rooms and take vital signs without human contact. And real dogs did their part, too! In Helsinki Airport, dogs were trained to sniff and screen passengers for COVID-19. That’s a good boy.

Reimagining the office
Needless to say, 2020 proved that the office as we know it might be less necessary than we thought. Workers flocked to video chat platforms like Zoom, while Twitter announced that its employees wouldn’t be forced to return to the office . . . ever again.
So what should we do with all of these vacant office buildings? As it turns out, there are a few excellent possibilities. We could turn them into affordable housing or we could turn them into schools. Either way, it certainly seems like a better option than putting up more cubicles.

Vaccine distribution
If there’s been one piece of good luck for us all during COVID-19, it’s that the vaccines are working better than most public health officials expected, not with the ~40% efficacy of a typical flu vaccine, but with 90%-plus efficacy.
Now the challenge is in distributing the vaccines as quickly as possible, and keeping them cold along the way. Pfizer’s vaccine, in particular, demands temperatures down to minus 80 degrees Celsius (that’s minus 112 degrees Fahrenheit) to stay viable—though the company is working on a powdered version to sidestep this issue. It’s a huge question of logistics. On this front, UNICEF’s work has been an inspiration, as it’s been building a map of cold-storage solutions to get the vaccine distributed across the developing world. And a company called Sure Chill has been providing countries with thousands of special vaccine refrigerators that can stay cold for days or even weeks without a source of power.

Meanwhile, in places like the U.S., we can learn a lot from how Amazon and Walmart ship and distribute products, leveraging our hyper-efficient supply chain for something that benefits public health instead of capitalism.
No, the list of innovations above wasn’t enough to stop the devastation of COVID-19, especially here in the U.S. But it’s encouraging to see that, even when the government failed to organize an adequate response, people have come together to build solutions themselves. Here’s hoping for a brighter 2021.
